Psoriasis is a condition which develop red patches of various sizes on the skin that are covered with dry, silvery scales.
Psoriasis is called as chhal rog in Hindi. In psoriasis the skin becomes inflamed and red eruptions appear on the surface of the skin that begin to itch excessively. These areas form thickened areas (plaques) that are covered with silvery scales over the reddened lesions. The skin at the joints may crack sometimes.
Psoriasis most often occurs on the elbows, knees, scalp, lower back, palms, and soles of the feet. The disease may also affect the fingernails and toenails. About 15% of people with psoriasis have joint inflammation that produces arthritis symptoms. This condition is called psoriatic arthritis.
Psoriasis is categorized as mild, moderate, or severe, depending on the percentage of body surface involved and the impact on the patient’s quality of life.
In some cases, psoriasis is so mild that is ignored by the patient in an early stage.
When it gets aggravated entire body get covered by psoriatic patches which give pain and excess itching, some time joint also gets pain in the early morning. Psoriasis affects between 2% percent of the general population. In the US alone there are about 5.5 to 6 million people suffering from psoriasis. Both males and females get psoriasis in equal numbers. It can strike at any age, but most often in adults between 15 and 35 years.
Pathology of Psoriasis
- Psoriasis is a chronic (long-lasting) skin disease characterized by scaling and inflammation.
-
- Our skin is mainly made up of two layers: epidermis (outer layer) and dermis (inner layer). The cells of the epidermis are borne in the dermis and then they move up. At a regular interval of 28-30 days, the cells of the epidermis are replaced by new cells formed in the dermis.
- In psoriasis, this process of cell production in dermis is sped up. New cells are formed and moved upward to the skin surface faster than they can be incorporated into skin. The excess cells accumulate and are scaled off in the form of flakes.
- Psoriatic plaque has other features also, including inflammatory cells and dilated small blood vessels that contribute to both the appearance and the symptoms of a psoriatic lesion.
Diagnosis of Psoriasis
In psoriasis red patches are develop in one or more area at the same time.to diagnose of psoriasis clinically is very much important. The white silvery scales of psoriasis are very distinctive and guiding feature for diagnosis. Also, consideration of the history, family history, the spread on affected areas, etc. is taken into account to conclude the diagnosis of psoriasis.
When psoriasis affects scalp patient may complain for excess dandruff in head. To diagnose psoriasis doctor must have a clinical eye to diagnose it perfectly.
- Patients family history (any person had psoriasis years before).
- History of auto-immune disease in the family to father mother, grandfather, grandmother, in-laws.
- How patients skin reacts to different seasons.
- Last medicine used and its effect on patches.
- At what time period or interval it gets the relapse.
- How it growing or what type of pathes he develops.
- Experirnced dr need just 5 minutes to diagnose psoriasis on this parameters after treating nosof cases of psoriasis.
Symptoms of psoriasis
In psoriasis the skin becomes inflamed and red eruptions appear on the surface of the skin that begin to itch excessively. These areas form thickened areas (plaques) that are covered with silvery scales over the reddened lesions. The skin at the joints may crack sometimes.
Psoriasis most often occurs on the elbows, knees, scalp, lower back, palms, and soles of the feet. The disease may also affect the fingernails and toenails. There are many variants and types of psoriasis. Although psoriasis may affect any area of the body, it is most commonly found on the scalp, elbows, knees, hands, feet, and genitals.
Types of psoriasis
Plaque psoriasis:
- Raised, inflamed, red lesions(plaques) covered in a silvery white scale.
- Typically found on the elbow,scalp,knees and lower back.However it apperarany where on the surface of the body.
- Plaques are typically itchy,sore(or both).
- Skin around the joints maycrck and bleed in severe case.
Pustular psoriasis:
- Pustules appear across a wide area of skin.
- Pustules develop rapidly.
- The pus is made upof white blood cells.
- The pus is not affected.
- Within a couple of days the pustules dry and peel off, after which the skin is shiny and smooth.
- Pustules may appear in cycles of weeks or even in few days.
- At the start of a cycle the patient may experience fever, chills, fatigue, and weight loss.
- Pustules may appear on the sole of feet or the palm of the hands.
- Pustules develop into round, brown, scaly sports.
Erythrodermic psoriasis:
- The most uncommon form of psoriasis.
- Whole body can be covered with a fiery red rash.
- There is usually intense itching.
- There is a typically an intense burning sensation.
- There is widespread inflammation.
- There is widespread exfoliation, during which time itching, burning and swelling is more severe.
Guttate psoriasis:
- Sometimes known as teardrop psoriasis or rain drop psoriasis.
- Plaques are usually small, No more than 1cm in diameter.
- Plaques are fairly widespread. They may develop anywhere in body, except the soles of the feet and palms of the hands. Most commonly it affects chest, arms, legs.
- Usually occurs after a step infection(throat infection) and is more common among teenagers and children.
- There is a good likehood that the Guttate psoriasis eventually disappear However some time youg patient also develop psoriasis.

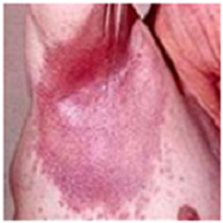
Inverse psoriasis:
- More common among over weight/obese individuals.
- As opposed to plaque psoriasis, inverse psoriasis is not characterized by scalling.
- Inverse psoriasis is characterized by inflamed, brightred, smooth pathes of skin.
- It can be very itchy or painful.
- If the skin rubs together in the folds, symptoms will be aggravated.
- Sweating in the skin folds may also aggravate affected areas.
- Most commonly affected areas include the armpits, groin, skin between buttocks and skin under breast.
- In obese patients, there may be symptoms under the belly.
The changes in the blood which lead to psoriasis are now also bringing changes in the joints, which could even be irreversible. Any joint could be affected in this process. The joint affection relatively becomes more difficult to treat. Interestingly, there is good treatment for psoriatic arthritis in homeopathy, especially if treated in the early stages.
Causes of Psoriasis
The exact cause of psoriasis is not fully understood. Cold climate and some form of injury can aggravate the problem. The recent discoveries point to an abnormality in the functioning of key white cells in the blood stream triggering inflammation in the skin. Because of the inflammation, the skin sheds too rapidly, every three to four days.
- Stress
- Food allergens
- Infections
- Environmental allergens
- Genetic tendency
- Drugs
- Systemic illness
- Skin trauma
Internal factors
Defective immune system: Recent research indicates that psoriasis is likely to be a disorder of the immune system. This system includes a type of white blood cell, called a T cell, that normally helps protect the body against infection and disease. Scientists now think that, in psoriasis, an abnormal immune system causes activity by T cells in the skin. These T cells trigger the inflammation and excessive skin cell reproduction seen in people with psoriasis.
Genetics and heredity: It is commonly seen that if any patient has psoriasis, there are chances that in his/her family one of person was suffering with psoriasis or may be with any auto-immune disease (maybe grand father, grand mother).
If any patient having psoriasis there is chances that his son/daughter develop psoriasis is 10%, instead of both are suffering with psoriasis chances of developing psoriasis is 30%. Researchers are studying large families affected by psoriasis to identify a gene or genes that cause the disease.
External factors
People with psoriasis may notice that there are times when their skin worsens, then improves. Conditions that may cause relapses of flare-ups include:
Climate:
Climate trigger psoriasis, cold temperature may aggravate psoriasis like anything where hot season reduces psoriasis.
Infections:
Both dermatological and systemic infections have been known to trigger the onset of psoriasis or a worsening of psoriasis.moslty viral upper respiratory disease, streptococcal pharyngitis (strep throat), and human immunodeficiency virus (HIV). Staphylococcal skin infections (boils) have been a trigger.
Stress:
Psychological stress is the cause as well as outcome of disease like psoriasis. It is a well-known fact that there is an inseparable bond between mind and body and psyche plays a vital role in maintaining health or causing diseases. It is a common experience in practice of patient reporting the onset of psoriasis following major stress like divorce, death of close relatives, change of job, unhealthy family relationships etc and this perception of patients that psychological stress can worsen psoriasis has been supported in clinical studies.
Certain medicines:
Certain medicines, most notably beta-blockers, which are used to treat high blood pressure, and lithium or drugs used to treat depression, may trigger an outbreak or worsen the disease. The drugs may be listed as: lithium, anti-malarials, mepacrine, NSAIDs, beta-blockers, alcohol.
Physical trauma:
People often notice new spots 10 to 14 days after the skin is cut, scratched, rubbed, or severely sunburned. Analysis of patient records has indicated that up to 50 percent of persons with psoriasis have had a ‘Koebner’s phenomenon’ experience – that is, have had a psoriatic lesion develop at the site of an injury or skin condition.